Page contents
The information here will help you understand your injury, guide you through your rehabilitation and explain what you can do to maximise your recovery.
Advice for a recent ankle injury
In the first 72 hours, it’s important to:
- rest your ankle
- elevate it above hip level
- apply a cold pack regularly
- use crutches and a boot for walking to protect your joint
It’s helpful to remember PRICER:
- Protect
- Rest
- Ice
- Compression
- Elevate
- Rehabilitation
Medication
The Emergency Department (ED) or a Minor Injuries Unit (MIU) may have prescribed you with some pain relief. Take these as instructed to help manage the pain.
If you do not feel that this medication is helping, talk to us during your appointment in Fracture Clinic, or your GP, about an alternative option.
Cold packs
Ice is a great natural anaesthetic that helps relieve pain and controls swelling. Apply ice packs or a bag of frozen peas wrapped in a wet thin towel to your injured area for up to 15 minutes every few hours.
- Do not place ice in direct contact with the skin.
- Do not leave the ice pack on for more than 20 minutes at a time in one hour.
Rest and elevation
It’s important to rest your injured area as much as possible in the first 24 to 72 hours.
It’s normal to experience swelling after your injury which is often worse at the end of the day.
Elevation reduces swelling, which in turn relieves pain and speeds up your healing. Keep your injured area elevated as much as possible during the first 24 to 72 hours.
If you have been given a sling, use it to keep your injured area elevated. You may find it more comfortable to use pillows to elevate it during the evening and at night.
If you have a lower limb injury, try to keep your feet elevated above the level of your hip.
Smoking
Medical evidence suggests that smoking prolongs fracture healing time. In extreme cases it can stop healing altogether. Stopping smoking during the healing phase of a fracture will help ensure optimal recovery from this injury.
For advice on stopping smoking and local support available, please discuss this with your GP or go to the NHS Smoke Free website.
Helping your recovery
Being healthy can help you recover from your injury faster. Eating well, staying hydrated and keeping as active as possible will all help. We’ve put together a set of videos on all the things you can do to help you recover as quickly as possible.
If you need an operation on your ankle
Sometimes an ankle injury may not heal by itself and you’ll need an operation to repair the break. Having an operation is always your choice and your surgeon will discuss the benefits and risks of surgery with you so you can make an informed decision. You can find out more about having an operation on your ankle on our surgery for fractures and soft tissue injuries page, and in this video:
Care plans
Below we have care plans for different types of ankle injuries, including information that will help you understand your injury, guide you through your rehabilitation and explain what you can do to maximise your recovery.
Your diagnosis should have been made by an orthopaedic consultant or one of the team working under the supervision of the consultant team. The information in these care plans is to help you understand your diagnosis and is not exhaustive.
Non-urgent advice: Please note:
Your consultant may give you a different, personalised care plan based on your injury and whether you need imaging (x-ray, CT scan, MRI, or an ultrasound) or an operation.
1. Soft tissue ankle injury / ankle sprain
What is your injury?
It’s a sprain to your ankle. This means you have damaged the soft tissue such as ligaments, tendons or muscles around the ankle joint. This can be graded from a mild sprain to a more severe sprain.
Healing
This injury normally takes up to 12 weeks to heal, but this may differ depending on your individual circumstances.
Follow up
Injuries like yours usually heal well on their own over time, so most people won’t need a follow-up. If you do, we’ll contact you by phone. A follow-up may be for physiotherapy or a clinical examination in Fracture Clinic.
Please contact the Fracture Clinic on 01872 253091 if:
- you’re unable to follow this rehabilitation plan
- you have any questions
- you’re struggling to remove your boot after 6 weeks
- you experience pain or symptoms other than at the site of the original injury or surrounding area
- you experience significant pain after 12 weeks.
Your rehabilitation plan
Your consultant or specialist may give you a different rehabilitation plan based on your injury and circumstances.
For the first 2 weeks after your injury:
- you can put weight through your injured leg
- early weight bearing (putting weight through your injured foot) helps speed up healing, so try to walk as normally as possible
- you may find it easier to use crutches in the early stages
- start the initial exercises straight away (labelled “Foot exercises”). Do these 3 to 5 times a day.
If you’ve been given a boot:
- wear it when standing and walking if needed – it will protect your ankle and make you more comfortable
- wear a long sock in your boot
- take the boot off at night, when resting at home and when doing your exercises.
Between 3 and 6 weeks:
- stop using the boot and walk without it around your house
- build up to walking without the boot when you go outside or for longer walks
- gradually increase your activity
- start the next set of exercises (labelled “Ankle stretches”).
After 6 weeks:
- resume day-to-day activities but respond to any pain you might experience
- avoid impact for 3 months (running, jumping and dancing)
- you might have mild symptoms for 3 to 6 months, especially after heavy tasks or long walks.
For more about your injury and demonstrations of the exercises
Watch this video about soft tissue ankle injuries from Brighton and Sussex University Hospitals.
2. Avulsion fracture
What is your injury?
You have a small break in one of 3 places:
- the outside of your ankle (a lateral avulsion fracture)
- the inside of your ankle (a medial avulsion fracture)
- your shin bone where it meets your ankle (an anterior tibia avulsion fracture).
Healing
This injury normally takes up to 12 weeks to heal, but this may differ depending on your individual circumstances. More severe avulsion fractures can take longer.
Follow up
Injuries like yours usually heal well on their own over time, so most people won’t need a follow-up. If you do, we’ll contact you by phone.
Sometimes however, an avulsion fracture may be more severe. If you have significant pain or swelling that is not settling after 4 to 6 weeks, please call the Fracture Clinic to book a face to face appointment on 01872 253091.
Please contact the Fracture Clinic on 01872 253091 if:
- you’re unable to follow this rehabilitation plan
- you have any questions
- you’re struggling to remove your boot after 6 weeks
- you experience pain or symptoms other than at the site of the original injury or surrounding area
- you experience significant pain after 4 to 6 weeks.
If you feel you’d like to see someone at any time in the 6 months after your injury, you can book an open appointment. Please call 01736 758892 to make an appointment.
Your rehabilitation plan
Your specialist may give you a different rehabilitation plan based on your injury and circumstances.
For the first 4 weeks after your injury:
- you can put weight through your injured leg – early weight bearing (putting weight through your injured foot) helps speed up healing, so try to walk as normally as possible
- you may find it easier to use crutches in the early stages
- wear your boot when standing and walking if needed – it will protect your ankle and make you more comfortable
- wear a long sock in your boot
- take the boot off at night, when resting at home and when doing your exercises
- start the initial exercises straight away (labelled “Foot exercises”). Do these 3 to 5 times a day.
Between 4 and 6 weeks:
- stop using the boot and walk without it around your house
- build up to walking without the boot when you go outside or for longer walks
- gradually increase your activity
After 6 weeks:
- start the next set of exercises (labelled “Ankle stretches”).
- you should not be using the boot
- resume day-to-day activities but respond to any pain you might experience
- avoid impact for 3 months (running, jumping and dancing, contact sports)
- you might have mild symptoms for 3 to 6 months, especially after heavy tasks or long walks.
For more about your injury and demonstrations of the exercises
Watch this video about avulsion fractures to medial navicular from Brighton and Sussex University Hospitals.
3. Undisplaced isolated medial malleolus fracture
What is your injury?
You have broken a bone on the inside of your ankle. This often involves some damage to the deltoid ligament which is also on the inside of your ankle.
Healing
This injury normally takes up to 12 weeks to heal, but this may differ depending on your individual circumstances.
Follow up
You’ll see a specialist 1 to 2 weeks after your injury and have a weight bearing (standing) x-ray. The specialist will explain the results and discuss the next stage of your care. There’s a chance that this fracture can move, or that it may not heal completely by itself, and you may need an operation. You can find out more about having an operation on your ankle further down the page.
We will follow up with you at 6 weeks and sometimes again at 12 weeks.
You can also book an open appointment at any time in the six months after your injury. Please call 01736 758892 to make an appointment.
Please contact the Fracture Clinic on 01872 253091 if:
- you’re unable to follow this rehabilitation plan
- you have any questions
- you haven’t heard from us about your follow-up appointment by 4 days after your injury
- you experience pain or symptoms other than at the site of the original injury or surrounding area
- you experience significant pain after 12 weeks.
Your rehabilitation plan
Your specialist may give you a different rehabilitation plan based on your injury and circumstances.
For the first 6 weeks after your injury:
- you can put weight through your injured leg – early weight bearing (putting weight through your injured foot) helps speed up healing, so try to walk as normally as possible
- you may find it easier to use crutches in the early stages
- wear your boot when standing and walking if needed – it will protect your ankle and make you more comfortable
- wear a long sock in your boot
- take the boot off at night, when resting at home and when doing your exercises.
- start the initial exercises straight away (labelled “Foot exercises”). Do these 3 to 5 times a day.
Between 6 and 12 weeks:
- stop using the boot and walk without it around your house
- build up to walking without the boot when you go outside or for longer walks
- stop using your crutches and boot (after 8 weeks)
- gradually increase your activity
- start the next set of exercises (labelled “Ankle stretches”).
After 12 weeks:
- resume day-to-day activities but respond to any pain you might experience
- avoid impact for 3 months (running, jumping and dancing)
- You might have mild discomfort and swelling for 6 to 12 months, especially after heavy tasks or long walks.
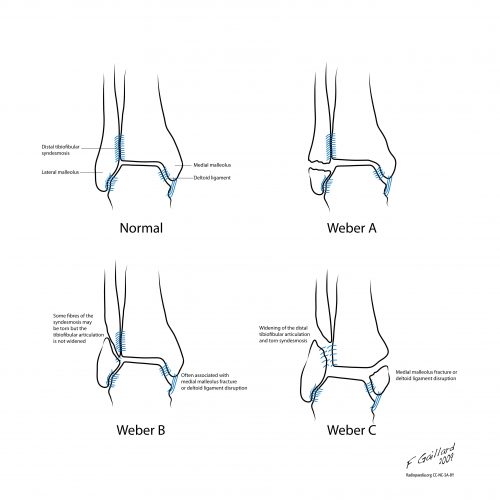
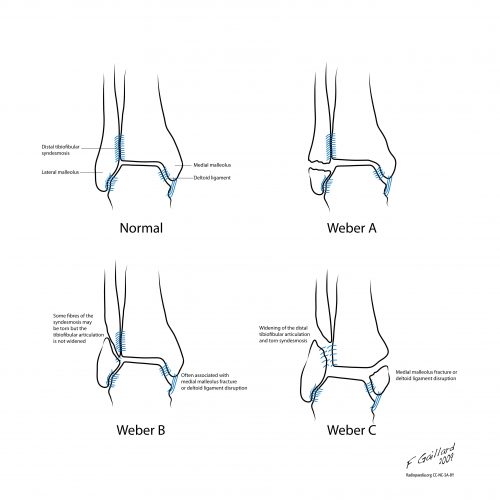
4. Weber A fracture
What is your injury?
You have broken a bone on the outside of your ankle (fibula).
Healing
This injury normally takes up 12 weeks to heal, but this may differ depending on your individual circumstances.
Follow up
Injuries like yours usually heal well on their own over time, so most people won’t need a follow-up. If you do need a follow-up or physiotherapy, we’ll contact you by phone.
If you still feel you’d like to see someone, you can book an open appointment at any time in the six months after your injury. Please call 01736 758892 to make an appointment.
Please contact the Fracture Clinic on 01872 253091 if:
- you’re unable to follow this rehabilitation plan
- you have any questions
- you’re struggling to remove your boot after 6 weeks
- you experience pain or symptoms other than at the site of the original injury or surrounding area
- you experience significant pain and stiffness after 12 weeks.
Your rehabilitation plan
Your specialist may give you a different rehabilitation plan based on your injury and circumstances.
For the first 4 weeks after your injury:
- you can put weight through your injured leg – early weight bearing (putting weight through your injured foot) helps speed up healing, so try to walk as normally as possible
- you may find it easier to use crutches in the early stages
- wear your boot when standing and walking if needed – it will protect your ankle and make you more comfortable
- wear a long sock in your boot
- take the boot off at night, when resting at home and when doing your exercises.
- start the initial exercises straight away (labelled “Foot exercises”). Do them regularly to get your movement back.
Between 4 and 6 weeks:
- try to stop using the boot and walk without crutches. Start walking around your house, then try outside
- wear your boot when you go for a long walk
- gradually increase your activity
- start the next set of exercises (labelled “Ankle stretches”).
After 6 weeks:
- your fracture should have healed
- resume day-to-day activities but respond to any pain you might experience
- avoid impact for 3 months (running, jumping and dancing)
- you might experience mild discomfort and swelling for up to 6 months, especially after heavy tasks or long walks.
- you might attempt the advanced balance exercises (1 and 2)
For more about your injury and demonstrations of the exercises
Watch this video about Weber A fractures from Brighton and Sussex University Hospitals.
5. Weber B or C fracture
What is your injury?
You have broken a bone on the outside of your ankle. In some cases, this can cause your ankle to become unstable.
Healing
It normally takes 8 to 12 weeks for your first symptoms to settle. It will likely take longer if you smoke or have diabetes.
You may need an operation to help your injury heal. A consultant will need to assess your injury and the stability of your ankle before making a formal recommendation on whether your injury should be managed with or without surgery. You can find out more about having an operation on your ankle further down the page.
You may have ankle pain and swelling for up to 12 months after your injury. Swelling is often worse at the end of the day. Taking pain medication, elevating your ankle and using ice or cold packs will help. There’s more information about this at the top of this page.
Follow up
You’ll see a specialist and have a weight bearing (standing) x-ray 1 to 2 weeks after your injury. There’s a small chance that this type of fracture can move. If it does, you may need an operation. We’ll discuss any further treatment, including surgery, with you at the Fracture Clinic when you have your x-ray. The decision to have surgery is always your choice.
You can also book an open appointment at any time in the six months after your injury. Please call 01736 758892 to make an appointment.
Please contact the Fracture Clinic on 01872 253091 if:
- you’re unable to follow this rehabilitation plan
- you have any questions
- you haven’t heard from us about your follow-up by 4 days after your injury
- you experience pain or symptoms other than at the site of the original injury or surrounding area
- you experience significant pain and stiffness after 12 weeks.
Your rehabilitation plan
Your specialist may give you a different rehabilitation plan based on your injury and circumstances.
For the first 6 weeks after your injury:
- you can put weight through your injured leg – early weight bearing (putting weight through your injured leg) helps speed up healing, so try to walk as normally as possible
- wear your boot when standing and walking – it will protect your ankle and make you more comfortable
- use crutches to take some weight off your foot
- wear a long sock in your boot
- take the boot off when resting at home and when doing your exercises
- you can also take the boot off at night, but if you get up to use the toilet in the night, it may be safer to sleep with the boot on
- start the initial exercises straight away (labelled “Foot exercises”). Do these 3 to 5 times a day.
After 6 weeks:
- start the next set of exercises (labelled “Ankle stretches”).
- we’ll tell you when you can stop wearing your boot but it will be at least 6 weeks
- gradually increase your activity but avoid impact activity for 3 months (such as running, jumping and dancing)
- You may have mild discomfort and swelling for 6 to 12 months, especially after heavy tasks or long walks.
For more about your injury and demonstrations of the exercises
Watch these videos from Brighton and Sussex University Hospitals:
6. Achilles tendon injury
What is your injury?
You have torn or ruptured the tendon at the back or your ankle.
Healing
This injury normally takes between 6 and 9 months to heal. Full rehabilitation can take more than 1 year, although there’s no guarantee that you’ll get back full function at the end of your rehabilitation.
After this injury, there is a 10-30% chance of re-rupture of the Achilles tendon over your lifetime. This happens because of repeated injury or stress to the tendon during healing. To help reduce the risk of re-rupturing your tendon, it’s very important that you follow this care plan and advice from your physiotherapist closely.
Follow up
A specialist physiotherapist will call you about a rehabilitation plan and explain how to adjust your boot. If you haven’t heard from us by 4 days after your injury, please call the Fracture Clinic. You may need an ultrasound. If you do, we’ll call you and ask you to come in.
If you are under 50 or biologically fitter, you’ll also need to be assessed urgently by a consultant or a member of the team in case you need an operation. These operations need to take place within 14 days of your injury. You can find out more about having an operation on your ankle further down the page.
Please contact the Fracture Clinic on 01872 253091 if:
- you’re unable to follow this rehabilitation plan
- you have any questions
- you do not receive your appointment details
- you’re struggling with your boot
- you experience pain or symptoms other than at the site of the original injury or surrounding area
You can also book an open appointment at any time in the six months after your injury. Please call 01736 758892 to make an appointment.
Wearing your boot
You will have been given a VACOped boot by the Emergency Department (ED) or Minor Injuries Unit (MIU). You can see how to fit your VACOped boot in this video.
The boot protects your ankle and will make you more comfortable. You must wear the boot all the time including in bed at night. Always wear a sock.
You’ll need to adjust the range of movement your boot allows in the weeks after your injury. Your rehabilitation plan below explains when and how.
Preventing a blood clot or Deep Vein Thrombosis (DVT)
You’re not allowed to do any exercises for a number of weeks. This puts you in a higher risk group for developing a DVT which can have very serious effects.
To reduce this risk, you have been prescribed a course of a blood thinner (anti-clotting medication). You’ll need to inject this at the same time every day for the first 4 weeks. We’ll show you how to do this.
If you have any questions about this, or if you have a reaction to the medication, please speak to your GP or district nurse.
You must dispose of your used injections safely into the yellow sharps bin provided. Once full, you can drop the sharps bin to the Fracture Clinic, your local Minor Injuries Unit or your GP practice where we can dispose safely of them.
Your rehabilitation plan
Your specialist may give you a different rehabilitation plan based on your injury and circumstances.
After your injury:
- wear the boot during the day and night
- remove your boot carefully for washing and to change your sock once a day. Whilst doing this, you must always keep your toes pointed down as shown in this picture. Do not flex your foot.

- do not stretch the calf or do any ankle exercises. This will disrupt tendon healing and your long term recovery.
- use your crutches and put some weight through your injured leg when you walk
- continue taking anti-clotting medication
After 2 weeks:
- adjust the range of your boot to between 20 and 30 degrees plantarflexion.
- This video shows you how to adjust the range of motion.
After 4 weeks:
- adjust the range of your boot to between 10 and 30 degrees plantarflexion.
- remove the boot throughout the day and gently move your ankle up and down within the range allowed by the boot. Do not push through any ‘stretch.’
After 5 weeks:
- keep the range of your boot between 10 and 30 degrees plantarflexion
- change into a flat sole
- regularly remove the boot throughout the day. Gently move your ankle up and down within the range allowed by the boot.
After 6 weeks:
- adjust the range of your boot between 0 and 30 degrees plantarflexion
- regularly remove the boot throughout the day. Gently move your ankle up and down within the range allowed by the boot
- rest your feet flat on the floor at an angle of approximately 90 degrees when sitting down
- smoothly and slowly raise and lower your heels whilst sitting
After 8 weeks:
- remove the boot at night
- try to gradually remove your boot during the day – this may take a week or two
- try walking short distances around your own home wearing a shoe
- wear bilateral heel raise pads, these should be given to you at the time your boot was issued or at a follow-up fracture clinic appointment.
- start ‘later rehabilitation’ in discussion with the physiotherapy team. We will guide you through this at the right time
- But do not start any exercises until you have been guided by your physiotherapist.
7. Distal fibula stress fracture
What is your injury?
You have a hairline fracture on the outside of your ankle. Stress fractures are often caused through overuse, with or without a subtle bio-mechanical problem. Pain will usually have developed gradually over time, rather than at a specific point in time.
Healing
This injury normally takes up to 12 weeks to heal, but this may differ depending on your individual circumstances.
We recommend you also see a physiotherapist for a thorough biomechanical assessment of the forces going through your lower limb to cause a stress fracture.
It is important to note that continuing the activity that caused the pain will not allow your injury to heal and REST must be part of your overall treatment plan.
Follow up
Injuries like yours usually heal well on their own over time, so most people won’t need a follow-up. If you do need a follow-up, we’ll contact you by phone. You may need physiotherapy, which can be organised through your GP or the Fracture Clinic.
If you still feel you’d like to see someone, you can book an open appointment at any time in the six months after your injury. Please call 01736 758892 to make an appointment.
Please contact the Fracture Clinic on 01872 253091 if:
- you’re unable to follow this rehabilitation plan
- you have any questions
- you’re struggling to stop using your boot after 6 weeks
- you experience pain or symptoms other than at the site of the original injury or surrounding area
- you experience significant pain after 12 weeks.
Your rehabilitation plan
Your specialist may give you a different rehabilitation plan based on your injury and circumstances.
For the first 6 weeks after your injury:
- you can put weight through your injured leg – early weight bearing (putting weight through your injured foot) helps speed up healing, so try to walk as normally as possible
- you may find it easier to use crutches in the early stages
- wear your boot when standing and walking – it will protect your ankle and make you more comfortable
- wear a long sock in your boot
- take the boot off at night and when resting at home
- start the initial exercises straight away (labelled “Foot exercises”). Do these 3 to 5 times a day.
After 6 weeks:
- stop using the boot and walk without it around your house
- resume day-to-day activities but respond to any pain you might experience
- build up to walking without the boot when you go outside or for longer walks
- start the next set of exercises (labelled “Ankle stretches”).
After 8 weeks:
- stop using the crutches
- gradually increase your activity but avoid impact for 3 months (running, jumping, plyometrics and dancing)
- You might have mild symptoms for 3 to 6 months, especially after long walks or heavy tasks.
For more about your injury and demonstrations of the exercises
Watch this video about distal fibula stress fractures from Brighton and Sussex University Hospitals.
8. Calf muscle tear
What is your injury?
Your calf muscle has been overstretched, causing micro tears to the muscle itself. This can range from mild to severe. It causes pain, bruising and weakness in the muscle. It may be difficult to bear weight on your leg.
Healing
This injury normally takes up to 12 weeks to heal, but this may differ depending on your individual circumstances.
It is important to avoid standing on your tiptoes for the first 6 weeks while healing is taking place.
Follow up
Injuries like yours usually heal well on their own over time, so most people won’t need a follow-up with orthopaedics. If you do, we’ll contact you by phone. We do recommend you see a physiotherapist. Your GP can refer you if we don’t follow up with you through the Fracture Clinic.
If you still feel you’d like to see someone, you can book an open appointment at any time in the six months after your injury. Please call 01736 758892 to make an appointment.
Please contact the Fracture Clinic on 01872 253091 if:
- you’re unable to follow this rehabilitation plan
- you have any questions
- you’re struggling to remove your boot
- you experience pain or symptoms other than at the site of the original injury or surrounding area
- you struggle to return to sport or exercise, or are still experiencing significant pain after 12 weeks
Your rehabilitation plan
Your specialist may give you a different rehabilitation plan based on your injury and circumstances.
For the first 2 weeks after your injury:
- you can put weight through your injured leg – early weight bearing (putting weight through your injured foot) helps speed up healing, so try to walk as normally as possible
- you may find it easier to use crutches in the early stages
- avoid standing on tiptoes
- start the initial exercises straight away (labelled “Foot exercises”). Do these 3 to 5 times a day.
If you’ve been given a boot:
- wear it when standing and walking – it will protect your ankle and make you more comfortable
- wear a long sock in your boot
- take the boot off at night, when resting at home and when doing your exercises.
Between 2 and 12 weeks:
- from 2 weeks onwards, start the exercises labelled “Balance strategy exercises 2“
- from 3 weeks onwards, start the exercises labelled “Ankle stretches“
- avoid standing on tiptoes until at least 6 weeks after your injury
- start walking without your boots and crutches around your house
- build up to walking without the boot and crutches when you go outside or for longer walks
- wear supportive shoes like trainers
- gradually increase your activity
- eventually stop using your boot and crutches
- you may still have some mild symptoms
For more about your injury and demonstrations of the exercises
Watch this video about calf muscle tears from Brighton and Sussex University Hospitals.
Boots, support straps, plaster casts and crutches
Using your boot
Your boot protects your ankle and will make walking more comfortable. It won’t heal your fracture but it will improve your symptoms.
Taking your boot on and off
Click on the image of your boot below to see a video showing you how to fit your boot.
Boot advice for people with diabetes
If you’re diabetic please contact the Fracture Clinic on 01872 253091 to discuss your boot. It’s especially important if you have problems with your skin. We can provide you with a specialist diabetic boot.
Footwear for the foot on your uninjured leg
Choose a supportive shoe or trainer with a firm sole for the foot on your uninjured leg. You’ll notice that your boot has a thicker sole. By matching this height on the uninjured side, you’ll reduce stress on your other joints.
You can buy an adjustable shoe balancer to match the height of your injured side.
Using your ankle support strap
We may have given you a strap to support your ankle, usually if you have badly sprained your ankle or after you’ve had an operation.
Using your crutches
These videos show you how to use your crutches.
What should I do with my boot, support strap or crutches when I no longer need them?
You can return crutches to the Fracture Clinic or your local physiotherapy department.
We cannot use boots or support straps again. You should not return them to the hospital.
If you’ve been given a plaster cast
For some ankle injuries the Emergency Department (ED) or Minor Injuries Unit (MIU) may fit you with a plaster cast. Keep this clean and dry. You can find out more about caring for your plaster cast here.
Preventing complications
Caring for your wound and stitches
If you’ve had an operation, you’ll need to keep your stitches dry and clean. You should also look out for any redness or signs of swelling, bleeding or pus as these can be signs of an infection.
You can find information about how to care for your stitches, if/when they need to be removed and signs of an infection on our surgery for fractures and soft tissue injuries page.
Blood clots and Deep Vein Thrombosis (DVT)
Because your limb is immobilised and you’ll be moving less than normal, you’re at higher risk of developing a blood clot or Deep Vein Thrombosis (DVT). This can be life threatening if left untreated.
Symptoms of DVT in the leg are:
- throbbing or cramping pain in 1 leg (rarely both legs), usually in the calf or thigh
- swelling in 1 leg (rarely both legs)
- warm skin around the painful area
- red or darkened skin around the painful area
- swollen veins that are hard or sore when you touch them.
These symptoms can also happen in your arm or tummy if that’s where the blood clot is.
More information about DVT
- Watch this video about how to prevent DVT.
- Learn more about DVT including symptoms, who is at risk and how to treat it.
- Find out how to reduce the risk of blood clots when you have an immobilised lower limb (PDF, 108 KB).
Preventative medication for DVT
If you have been told not to put any weight through your leg or to partially weight bear (50%), you should have been assessed in ED or MIU and told if you need to take preventative medication.
If you have not had this conversation please call your GP for an urgent appointment.
Depending on your injury, you may have been prescribed a course of a blood thinner. There are a few different types of medication and they often need injecting into your tummy. You can discuss an alternative with a doctor. Please see the relevant care plan for your injury.
Pressure sores and ulcers
Wearing a boot or plaster cast combined with not moving your limb can lead to pressure sores or ulcers. These are injuries to the skin and underlying tissue caused by prolonged pressure, rubbing or tension.
They often develop gradually, but can sometimes form in a few hours.
Signs and symptoms of pressure sores
These include:
- skin discolouration – red patches for people with pale skin, purple or blue patches for people with dark skin
- discoloured patches that do not turn white when pressed
- a patch of skin that feels warm, spongy or hard
- pain or itchiness in the affected area.
If you have a boot, take it off every day to check your skin and make sure it’s not rubbing.
If you have a plaster cast, look out for a change in colour (red or white) of your skin above or below the plaster, an increase in pain inside the plaster or pins and needles.
- Watch this video to learn how to prevent pressure sores.
- Read more about pressure sores on the NHS website.
If you think you have a pressure sore or ulcer call the Fracture Clinic straight away on 01872 253091.
For out of hours advice please call 01736 758909.
Sepsis
Sepsis (also known as blood poisoning) is a serious infection that can be life threatening. There is no one sign for sepsis so it can be hard to spot.
Call 111 immediately if you develop any of the following:
- Slurred speech or confusion
- Extreme shivering or muscle pain
- Passing no urine in a day
- Severe breathlessness
- It feels like you’re going to die
- Skin is mottled or discoloured.
Find out more about the symptoms of sepsis on the NHS website.
These videos also explain what sepsis is and how to spot the early signs.
Living with your injury
Work
Decisions to return to work are made on a unique basis and should be discussed with the Fracture Clinic, your GP, and your employer.
You may need time off work and when you return, you may need light or amended duties. When you should return to work will depend on your profession and your injury.
If you see us in person at the Fracture Clinic we can give you a fitness for work statement or a sick note. If you don’t come to see us, you can also get one from your GP.
Driving
If you have an injury to a lower limb (foot, ankle, or knee), you can return to driving when you:
- have been told you no longer need your brace, boot or crutches, or your plaster cast has been removed
- can walk comfortably
- can perform an emergency stop pain-free.
Always test your ability to drive with the ignition off and in a safe environment.
If you have a follow-up appointment with us, please wait until your consultant or physiotherapist has given you clearance to drive.
If you’re in any doubt, do not drive until you have spoken to our team.
Sport
You should not do any sports at all for at least 6 weeks.
You must avoid impact sports, jumping, running, dancing, and heavy lifting for at least 12 weeks.
Some injuries will mean you have to wait longer before you can return to sport or impact activities. Please check your specific care plan. If you’re unsure about whether you should do a sport or activity, please call the Fracture Clinic on 01872 253091.
Thank you to Brighton and Sussex University Hospitals for kindly letting us use information from their care plans to create this site.
Page last reviewed: 5 January 2024