Page contents
If you have fallen and fractured your hip, you’ll need an operation to repair it. If you have hip degeneration and have chosen to have surgery to reduce ongoing pain, you can find out more about your planned hip replacement operation.
The information here will help you understand your injury, guide you through your rehabilitation and explain what you can do to maximise your recovery after hip fracture surgery.
About your injury
What is your injury?
You have fractured your hip at the top of your thigh bone where the ball and joint socket meets your pelvis.
You might hear a hip fracture described as a ‘fractured neck of femur’ or a ‘fracture of the proximal femur’.
About your hip operation
You have had one of the following operations, depending on where you’ve broken your hip.
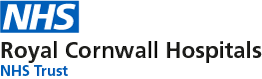
Dynamic hip screw operation (DHS)
You have had a dynamic hip screw device (DHS) inserted to hold your broken thigh bone together while it heals.
A DHS is a fixation screw and plate which treats a fracture to the neck of your femur. It will stay in place permanently, even after your fracture has healed.
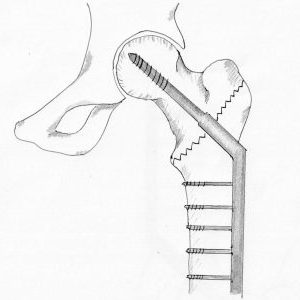
Hemiarthroplasty operation
You have had a hemiarthroplasty operation to replace one half of your hip joint (head of the femur or ‘ball’ part of the joint). The socket part remains intact.
This operation happens if your fracture damages the head of the femur. We will remove the fractured head of the femur and replace it with a prosthesis or artificial component.
Follow up
Most patients will not need a follow-up appointment after surgery. We’ll tell you when we discharge you from hospital if we need to see you again or if we feel you may benefit from further physiotherapy input.
Please contact the Fracture Clinic on 01872 253091 if:
- you’re unable to follow this rehabilitation plan
- you have any questions
- your injury becomes more painful
- you notice pain in an area other than your hip.
Healing
The bones, soft tissues and muscles surrounding your hip will take time to heal. It’s important to take extra care for the first few weeks following your operation.
Advice for recovering
- Take regular rest periods each day
- Aim to be as active as you can within the limits of your pain
- Be aware of increased pain and swelling related to increasing your activity levels
- If you experience sharp pain stop immediately
- If symptoms persist contact your GP.
What to expect after your operation
We encourage you to move as soon as possible. Make sure you take pain relief to help you to do this.
The day after your operation
We’ll help you sit out of bed and walk using a walking aid. This will reduce your risk of a blood clot or deep vein thrombosis (DVT) which can happen when you move less than normal after surgery.
If you’ve had a dynamic hip screw operation, your medical team will tell you how much weight to put through your leg on your operated hip. Your physiotherapist will show you how to do this safely before we discharge you.
If you’ve had a hemiarthroplasty operation, you can put as much weight as you can tolerate through your operated leg unless we tell you otherwise. Your physiotherapist will teach you how to do this safely before we discharge you.
It is very normal to feel less confident after a hip fracture and hip surgery. It takes time for surgical pain to ease, swelling to go down, the bone to heal and to recover strength.
Leaving hospital and returning home
You may be able to return to your own home or you may need to stay with family or friends. Your doctor and physiotherapists will discuss this with you and help you decide depending on:
- your home situation
- the amount of home assistance you have
- the rate of your progress
- your physical condition.
We’ll give you crutches or a frame to help you walk at home. We may also refer you to physiotherapy as an outpatient, if we feel this will benefit you.
Managing your injury at home
Pain and swelling
After your operation, you may feel some pain for a few weeks. Use this to guide you when increasing your daily activities.
You may have swelling in your leg for up to 3 months after your operation. Resting on a bed with your legs raised for a few hours each day will help you manage it.
What happens if the swelling gets worse?
The swelling may be quite severe and you may also feel it in your foot and ankle. This is very common. The blood thinning medication, which reduces your risk of developing blood clots in your leg, can cause more severe swelling.
You may need to stop taking the medication for a few days. Check with your GP or the Fracture Clinic before you do this.
Severe swelling may cause your skin to blister. If that happens, contact your GP or the Fracture Clinic immediately.
Signs of infection
If the area around the wound becomes red, gets more painful, discharges pus or you feel unwell with a high temperature, call 111 immediately. There’s more information about signs of infection and sepsis in the preventing complications section further down this page.
You can also read our patient information leaflet about managing a fracture related infection.
Early movement
Early movement will help your injury heal and prevent further complications such as deep vein thrombosis (DVT).
When you get home you’ll be able to:
- walk with a frame or crutches
- get on and off the bed
- carry out a home exercise programme.
You may be able to use the stairs. We will have practised this with you in hospital to ensure your safe discharge back home.
Washing and dressing
It’s best to wash and dress sitting down. Wear loose clothing for ease and comfort.
Your occupational therapist (OT) will explain the best way to do this and give you any equipment you need while you’re in hospital.
Walking
Use your frame or crutches until you can put your full weight through your injured leg and feel confident to move without them.
When you can put your full weight through your leg, you may walk with a limp due to muscle weakness in your hip. If you’re limping, keep using your walking aid until it improves. The exercises below will help strengthen your hip.
Some people may always need a walking aid.
Watch these videos on how to walk with crutches.
You can start to gradually increase the distance you walk each day after 2 weeks.
Walking up and down the stairs
Take one step at a time. Hold onto the handrail if you have one. We’ll show you how to manage stairs before you leave the hospital.
Take both crutches in your other hand as shown by your physiotherapist.
Watch these videos on how to walk with crutches including how to walk up and down the stairs and follow the instructions below.
Walking upstairs
- Hold onto the handrail
- Step up with your unoperated leg first
- Step up with your operated leg
- Bring your crutch up to same step as both legs

Walking downstairs
- Hold onto the handrail
- Place your crutch down one step
- Step down with your operated leg
- Step down with your unoperated leg.

Standing up and sitting down
Watch these videos on how to stand up and sit down using crutches and follow the instructions and pictures below.
Standing up using crutches
- Shuffle to the front of your chair and tuck your feet underneath you
- Put your operated leg out in front of you for comfort
- Push up with both hands on the arms of the chair, or push up with one hand on the arm of your chair holding your crutches in the other hand
- Once you feel balanced, put both hands in your crutches


Standing up using a frame
- Push up with both hands on the arms of your chair
- Once you feel balanced, hold onto the frame
Do not use the frame to pull yourself up.


Sitting down using a frame or crutches
- Stand close enough to feel the chair against the back of your legs
- Either let go of the frame and reach back to the arms of your chair with both hands, or place both crutches in one hand and place the other on the arm of your chair.
- Step your operated leg forward and gently lower yourself into the chair.
Do not sit down with your hands still on the frame or crutches.
Exercises
These exercises will help strengthen your hip and maximise your recovery.
Exercises to do in the first week after your operation
Start these exercises the day after your operation.
Try to do 10 of each exercise on both legs, 4 times a day. Your physiotherapist will show you how to do them.
Static quads
- Lie or sit on a bed with your legs straight
- Pull your toes up towards you, then tighten the muscles in front of your thigh pushing your knee down into the bed
- Hold for 5 to 10 seconds.

Static glutes
- Lie on your back on a bed with your legs straight
- Squeeze your buttocks firmly together
- Hold for 5 to 10 seconds and then relax.

Hip flexion/heel slide
- Lie on your back on a bed with your legs straight
- Slide the heel of your operated leg towards your bottom allowing your knee to bend
- Slide it back down again.
Use a plastic bag underneath your heel. This will stop any friction.

Sitting exercise to strengthen your muscle in your thighs (long arc quads)
- Sit on a chair with your feet on the floor
- Straighten your knee using the muscles in the front of your thigh
- Hold your leg out straight for 5 seconds then slowly return your foot to the floor.
- Try to ensure you sit up nice and tall to engage your tummy muscles as well.

Exercises to do after one week
After a week, you should be mobile and comfortable using your frame or crutches.
Make sure you hold onto a firm surface for all standing exercises.
Do 10 of each exercise, 4 times a day.
Hip flexion
Use a chair to support yourself.
- Slowly lift the knee of your operated leg up towards your hip height.
- Lower your leg back down to the floor.

Lying hip abduction
- Lie on your back with your legs straight.
- Keep your leg straight and your toes pointing to the ceiling
- Slide your leg out to the side as far as comfortable
- Return your leg to the centre.

Hip extension
Do this exercise ONLY if you’ve had a DHS operation.
Use a chair to support yourself.
- Keep your body upright
- Slowly move your operated leg back as far as possible
- Return your foot to the starting position.

Hip abduction
Do this exercise ONLY if you’ve had a DHS operation.
Use a chair to support yourself.
- Keep your body upright
- Keep your toes pointing forward and lift your operated leg out to the side
- Return to the starting position.

Exercises to do after 2 weeks or when you feel able to do so
You can try the following exercises if you feel able to. If you feel they’re too difficult, either miss them out or come back to them at a later stage.
Gradually increase the distance you walk each day. If you feel able you may wean yourself off your walking aids, but we recommend using them if you still have a limp.
Hip abduction
Do this exercise after 2 weeks ONLY if you’ve had a hemiarthroplasty.
Use a chair to support yourself.
- Keep your body upright
- Keep your toes pointing forward and lift your operated leg out to the side
- Return to the starting position.

Supported calf raise
- Stand and hold onto a firm support such as the top of a bench, back of a chair or stair rail
- Slowly rise up onto your toes lifting your heels off the ground
- Lower yourself back down with slow and controlled movements
- Repeat 20 times, 3 times a day.

Single leg balance
- Stand and hold on to something firm such as a chair
- Take all your weight on your operated leg. Try to lift your other leg off the ground.
- Hold for as long as you are able, gradually building up to 30 seconds.
- Repeat up to 5 times.
To make this harder, try to let go of your support only if you feel safe to do so.

Half squat
- Stand with your feet hip width apart.
- Hold onto a support such as the back of a chair
- Bend both knees as far as it’s comfortable and then push back up to straighten them
- Repeat 10 times.

Bridge
- Lie on your back with your knees bent and your feet hip width apart
- Push down through your feet, squeeze your buttocks and lift your bottom up as high as you can. Make sure your knees don’t start to fall out to the sides.
- Hold for 5 seconds and then lower down gently
- Repeat 10 times.


Preventing complications
Once your wound has completely healed you can massage gently around the scar to prevent permanent scarring. Massaging scar tissue can improve the healing of the wound site and break down scar tissue which can become painful.
Use your thumb to make small circular movements along and around the scar. You can use an oil or an unperfumed body lotion to do this. Please talk with your physiotherapist if you’re unsure and they can show you how to perform scar massage.
Living with your injury
Work
Decisions to return to work are made on a unique basis depending on your particular job role and operation and should be discussed with the surgeon, your GP and your employer.
You may need time off work and when you return, you may need light or amended duties. When you should return to work will depend on your profession and your injury.
You can get a fitness for work statement or a sick note from your GP or before you leave hospital.
Driving
You can return to driving when:
- you’re fit enough to do an emergency stop
- you’re nearly pain free
- you no longer depend on walking aids
- you have a good range of movement
- you have confirmed it’s okay to drive with your insurance company.
You can usually drive 6 weeks after your operation. If you have an automatic car and have injured your left leg, you may be fit to drive sooner. However, you must let your insurance company know that you have had an operation as insurance can be invalid according to each insurance company.
Always test your ability to drive with the ignition off and in a safe environment.
If you’re in any doubt, do not drive until you have spoken to our team.
Sports and hobbies
We recommend low impact activities such as walking or gardening. When you feel you can get into the pool safely, you can return to swimming.
You should avoid high impact activities and heavy lifting until at least 12 weeks after your operation.
Page last reviewed: 10 May 2023